adventures with my 90+ year old Bladder
Updated through June, 2023
|
Dear Friends,
This tale seems to have turned into: - a Shaggy dog story - an endless pointless tale intended be be a disappointment - The Perils of Pauline Sorry about that. |
Table of Contents
- Background - 2016
- Adventure at Stanford Medical. Honeymoon period - Monday Oct 22, 2018
- Adventure at Stanford Medical. Honeymoon is over - Tuesday October 23, 2018
- Comments from the Doctor's Office - October 24, 2018
- Comments from Others - October 25, 2018
- Removing the 2nd Foley - October 29, 2018
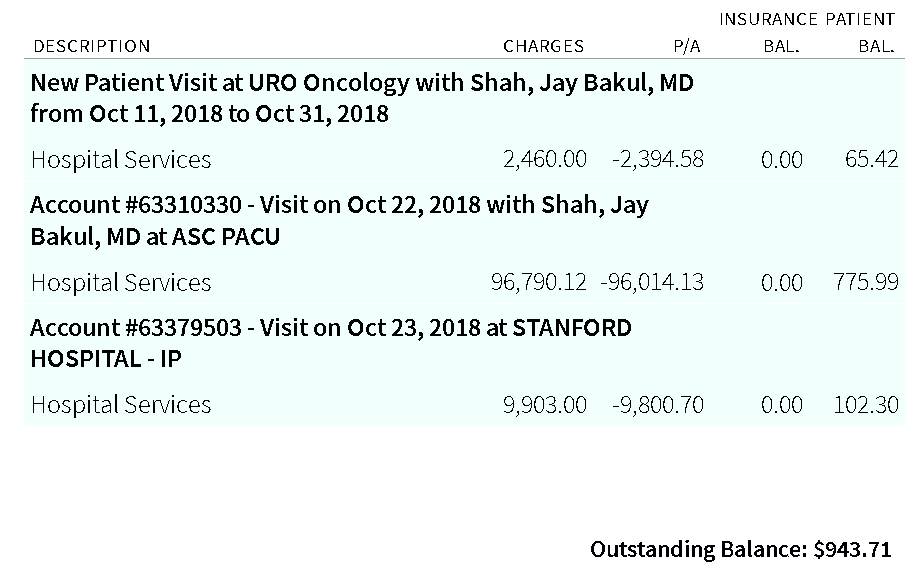
- The Bill !! - I would expect a bill like this for open heart surgery - Jan 11, 2019
- Cloudy urine - March 2019
- The Saga Continues ... - May 2023
|
After finding trace of blood in my urine, a cystoscopy was ordered and performed.
The Dr. found "small" patch of white with little projections. The surgeon thought it best
to get tools in there and check it, and while he was in there, scrape the middle lobe of my
5x sized prostate.
So a week later a later, the Dr. performed a "procedure" in a surgical center across the bay "resecting" the tumor.
A thick catheter hung from my "private" parts which connected to a black rubber thingy with three outlets. I have pictures, but they are too gross even for me :-(( Foley catheter
Everything was so-so until I got home. (The wife was driving). I had just gotten into the house when AN ENORMOUS PAIN GRABBED my bladder area. I could barely get to a chair to collapse. The pain was even worse than a steam burn I got 50 years previous.
I wanted to go to a local Emergency Room to stop the pain.
But I thought I couldn't walk reliably to the car. We called 911.
By the time they arrived (a fire truck arrived first :-) the pain was less
but I have a 911 ride to a local Emergency Room (ER).
A doctor at the ER ordered a shot of morphine (Hey, that stuff REALLY works :-)
then asked if I had taken my bladder anti-spasm pills.
After maybe a week, I went back to the local unmentioned provider to have that the monster catheter three way thingy removed.
|
Another cystoscopy at the unnamed medical service in October 2018
Adventure at Stanford Medical. Honeymoon period - Monday Oct 22, 2018
|
I didn't want another bladder surgery at the unnamed institution.
The new urologist referred me to a Dr Shah at Stanford Medical.
I looked up Dr. Shah, impressive, an associate professor, lots of medical papers.
During the introductory visit I offer to show him my home movie of the previous exam.
Dr. Shah said he prefered to read the report.
I ask that he prescribe an anti-bladder spasm drug so I don't get nailed as happened last time.
Next visit is the pre-op - yes, I'm alive (good vital signs ;-)
Planning
|
Adventure at Stanford Medical. Honeymoon is over - Tuesday October 23, 2018
|
As mentioned above, at 8 AM I am in happy land - no pain, no pain pills, catheter out, free as a bird, feeling great. The "kids" call on a linked line,
and I give a happy, glowing report :-)
About 2:00 PM I wonder why I haven't had the urge to pee. So I try - nothing happens. About 3:00 PM I decide to go poop and see if that will start the pee. Only poop - The instructions say if questions/problems call nnn before 5, and after 5 the Emergency Room at another phone number. So at 4:30 PM I call the first number, and am told the staff leaves at 4:30 and has left. The operator transfers me to the Emergency Room number - long wait -. The ER says they will call a Dr. who will call me. About 5:30 a Dr. calls - says he can meet me at ER at 7 PM. I head across the bay (against the commute :-) and arrive at 6:20. Get ticket from valet parking in front, advised that if I get it stamped parking will be free. By say 6:30 I'm registered (they said there was a call ahead about me arriving) and start sitting. At about 7 PM I mention to the Visitor Assistant that a doctor was supposed to meet me "here" at 7 PM. At 8 PM I tell the Visitor Assistant that I could be waiting at an ER much closer to home and that I plan to leave in ten minutes. Eight minutes later I am summoned and taken back to a comfortable leather chair (no arms) in a curtained area with patients about (I think location D10). About 8:30 I get a little urge to pee, and am shown a toilet. I go in, lean over the toilet and WOW I HURT. I pee some into the toilet but am covered all over with sweat - I pull the Emergency Cord and assistant hurries in - by then I have my head on some supporting bar, and feeling faint. Assistant gets a rolling chair and gets me to a bed in D10. She sees my sweat soaked shirt and gets me a hospital robe and warm thin blankets. I kinda am confused, but about 10:30 Dr. "Calab" shows up, inserts another "Foley", sends a prescription for "TAMSULOSIN 0.4 MG CAPSULES" describing this as an "Alpha blocker" that should ?relax me and promote peeing. I head for home about 11:00. I go to sleep in my recliner. Wednesday Oct 24th, no fun, Kinda hurt, and if I move, the Foley thing shifts in my insides and was really unpleasant. A neighbor nurse came over and asked if she could look. Anything ! "Oh, this isn't right at all! Who did this?" I told her a Stanford doctor. She said something like "Doctors should do things they know - This is work for nurses, we know about these thing." Then she showed Betty that a little clamp was not holding the hoses properly. Then she said "There should be a tube between the Foley and the bag. Did you take it out?" No way, I touched nothing - She said I should go to some facility and get a tube, and that the bag should be attached to the lower leg, not the thigh. So I go to the local Kaiser ER. The entry person says that they are very busy, but fixes an wrist band, and I wait. After two hours I say goodbye and head for the local PaloAlto Medical - In 10 minutes a sympathetic male nurse says he can fix it but needs a Dr's instruction to do it. In another ten minutes the tube is added and the bag tied to my lower leg, and most of the discomfort is gone, gone, gone :-)
In case you think I've been too detailed, you are correct - but I left a lot out. |
Comments from the Doctor's Office - Wednesday October 24, 2018
|
Dear Mr. Thelen,
I hope you have been recovering well since the procedure to resect your bladder tumor. I heard about the need to have the Foley catheter put back in. That is not uncommon in men in your age group. I am optimistic you will be peeing normally soon. The pathology report from your operation Monday shows that you had the lowest stage, lowest grade bladder cancer recurrence possible. There was muscle present in the specimen and it was NOT involved with cancer. This is very encouraging news! To check for recurrence, you need to have someone look in your bladder every 3 months from now on. You can have it done with Dr. Shinghal or you can contact my clinic to make an appointment with my team. Dr. Shinghal and I have a great working relationship and I am comfortable with you having your cystoscopy with either of us - go with whatever is easiest for you. Thank you for entrusting me and my team with your medical care. Please reach out to us if you have any questions. We wish you good health! Sincerely, Jay Shah, MD Associate Professor, Department of Urology Stanford University School of Medicine PS, sorry to reach out to you over MyHealth instead of the phone. I am currently traveling for work and I did not want you to have to wait until I got back to get the results. Study Result Narrative Accession No: SHS-18-38365 SPECIMEN SUBMITTED: A. POSTERIOR BLADDER WALL B. BLADDER NECK AND PROSTATE DIAGNOSIS: A. URINARY BLADDER, POSTERIOR, TRANSURETHRAL RESECTION - PAPILLARY UROTHELIAL CARCINOMA, LOW-GRADE, NON-INVASIVE (SEE SYNOPTIC TABLE) -- LAMINA PROPRIA AND MUSCULARIS PROPRIA ARE BOTH PRESENT AND UNINVOLVED BY TUMOR B. URINARY BLADDER NECK AND PROSTATE, TRANSURETHRAL RESECTION -- PROSTATE WITH NODULAR HYPERPLASIA ROJANSKY/RICHARDS/KAO COMMENT: Please see synoptic table below for more information on the bladder tumor: URINARY BLADDER: Biopsy and Transurethral Resection of Bladder Tumor (TURBT) SPECIMEN Procedure: TURBT TUMOR Tumor Site: Posterior wall Histologic Type Papillary urothelial carcinoma, noninvasive Histologic Grade: Low-grade Tumor Extent Tumor Extension: Noninvasive papillary carcinoma Accessory Findings Tumor Configuration: Papillary Muscularis Propria Presence: Muscularis propria (detrusor muscle) present Lymphovascular Invasion: Not identified PATHOLOGIC STAGE CLASSIFICATION (pTNM, AJCC 8th Edition) Primary Tumor (pT): pTa: Noninvasive papillary carcinoma CLINICAL HISTORY: Bladder cancer OPERATION: TURBT with blue light GROSS DESCRIPTION: Two specimens are received labeled with the patient's name and medical record number. The first specimen labeled "posterior bladder wall" is received in formalin and consists of three soft pink to tan papillary tissue fragments that aggregate to 1.4 x 0.8 x 0.6 cm. The specimen is entirely submitted in one cassette labeled A1. The second specimen labeled "bladder neck and prostate" is received in formalin and consists of 2 g of multiple rubbery pink focally nodular tissue fragments that aggregate to 3 x 2.2 x 1 cm. The specimen is entirely submitted in two cassettes labeled B1 and B2. Singel (10/22/2018) I have reviewed the specimen and agree with the interpretation above. CHIA-SUI KAO, M.D. Electronically signed 10/24/2018 5:41 PM |
Comments from Others - October 25, 2018
from Carl, another retiree
|
Removing the 2nd Foley - October 29, 2018
|
So, after the Monday Morning Commute, I drive to the 5800 Hollis Street Emeryville Stanford Medical facility - 30 miles away - arriving
before the 11:30 appointment.
They use valet parking (that causes its own complications later.) Everything goes smoothly. The game plan is to back-fill my bladder with 250 cc of fluid to help me pee soon. Then the operator (Physician's Assistant or nurse or ...) says that I should blow out. I finally understand that she means like blowing out candles - so I "blow out" and she quickly pulls out the Foley. She agrees that the idea was to distract me and keep me from fighting (flinching/tightening_up) the removal. Now the plan is for me to pee - and if I can't pee another Foley goes in for another week - No way, I privately plan that if I can't pee to escape and take my chances locally again. The thought of another week with an accursed Foley makes me desperate. Life is too short for that crap. So I wait ... that assistant pops in on a ten minute basis to check progress. Every little while I try to pee - but it hurts and I flinch, but I think the flow started, but it didn't - nothing - After about two hours I decide that maybe a going to a bathroom setting and pooping will get my brain in order and I maybe will really pee. I successfully poop, but get dizzy and feel faint. I think I got back to the room under my own guidance - but then I really feel faint. I call the assistant for help - she takes my blood pressure - it was less than 80 over 50 ? - from my normal 130/90 - I can barely see.
They talk of something that sounds like Vagovagal reflex
or Vasovagal response -
I'm not really clear about this ...
I try to fight this weakness flexing arms and lifting feet - when I talk I sound to myself like I am in another room - for a short while the back of my hand seemed orange and purple. After an unknown time interval, they call 911 - and the people in blue attach another set of electrodes ... They suggest that they take me to a hospital that I don't know - I ask to go to a Kaiser institution because Kaiser has records on me. By now I am up to feeling weak and wobbly, but think I can make "wise cracks". Folks are polite. About 4:30 I am in Kaiser Oakland, room C15. Dr. Middleton prescribes 2 liters of IV fluid. I would like to object, that I drink water like a fish, and that I am not dehydrated, but fortunately keep my mouth shut.
Time passes and passes - about 8:30 I finally pass about 150 cc of urine, less than the
the amount pre-set into my bladder so many hours ago - what the heck ??
BUT - by now the Emeryville Stanford valet parking has closed for the day - what to do?
I call another son, Carl, who lives a few miles north of Oakland Kaiser. Carl arrives and gets to chatting with Dr. Middleton who comes from the hills of Tennessee - good for a lot of kidding - They have a good time - Carl then takes me home -
Next day, Tuesday, I must recover the car from Emeryville valet parking.
Wife Betty sets up the trip with Uber, about half the price of a cab which wants $3/mile -
My car is parked right by the check-out stand. - The valet folks remember me being hauled out on my back and are happy for me. "All's well that ends well" :-) |
|
Cloudy urine - March 11, 2019 - (last "normal" test was Aug 2016, all since have had Abnormal flags)
|
URINALYSIS AUTO W/O SCOPE -
About This Test
If you have questions or concerns regarding your test results, contact the clinician who ordered the test.
|
The Saga Continues ... - May 2023
|
Happily, life returned to "normal" -
The exceptions being that
By early May the interval was about 90 minutes, and annoyingly also had to "defecate" - "poop" in street talk. This makes normal civilized life, visiting, going to restaurants, etc "inconvenient". Also a "good night's sleep" is a thing of the past. By mid May, I was sleeping in a recliner (quicker up to the toilet) and losing patience. Let's not mention defecating each time (very little) and wiping up way too often !! Like frequently rubbed skin gets really sore - Couldn't get a timely appointment with my urologist (3 week wait), so on May 20th I went to the Kaiser Emergency Room - got moved to the hospital were the next day a Foley catheter was inserted.
What a blessing!!
Had appointment with my regular urologist June 1st, 8:30 AM appointment for removal of the catheter. trying to pee, forgot how??
By 3:00 I had not peed and was beginning to feel "full". I call and was told to come in.
Dr. said that options were surgery or catheter. To me, surgery at my age seemed a poor idea, so I will change Foley catheters every 4 weeks. After inquiries about any allergy to latex, a new Foley was inserted. After about 48 hours the urine color finally went from strawberry to light pink. |